Share
What impact does development of cataracts have on someone already living with glaucoma?
Now I have cataracts as well! After grappling with a diagnosis of glaucoma, understanding the aims and choices of treatment, you have been told that you have cataracts. A cataract is the process by which your natural focusing lens changes from being transparent to being cloudy.
Glaucoma is usually asymptomatic: it is called the "sneak thief of sight". By contrast, cataracts often do have symptoms that may impact on your quality of life. The symptoms of cataracts, vary with the type and location of the lens opacity you have. Commonly patients complain of decreased central vision. This is noticed especially when driving and looking out into the distance. The letters on the eye chart appear smudged and indistinct. They are not missing or distorted as occurs with macular degeneration. Often the vision may be improved by looking through a pinhole. This may not be the case if the cataract is very dense.

Sometimes debilitating glare may be the main (or even the only) symptom. The cataract can scatter light as it passes through the eye resulting in glare effects. These are often most bothersome at night, especially from oncoming headlights when driving. As cataracts often take a long time to develop, the visual loss may be gradual and attributed to "normal aging". Once the cataracts or one cataract is removed, people are able to appreciate the visual decline that the cataract had caused.
Cataracts are more common in patients with glaucoma. Both conditions are increasingly common with age. Glaucoma associated with pseudo exfoliation (PXF), inflammation such as uveitis, and acute angle closure can predispose a person to the development of cataract. The treatments used for glaucoma, primarily drops, laser and less commonly trabeculectomy surgery can also accelerate the formation of cataract. Steroids in the form of eye drops, tablets, creams and even puffers can increase the pressure in the eye as well as accelerate the formation of cataracts.
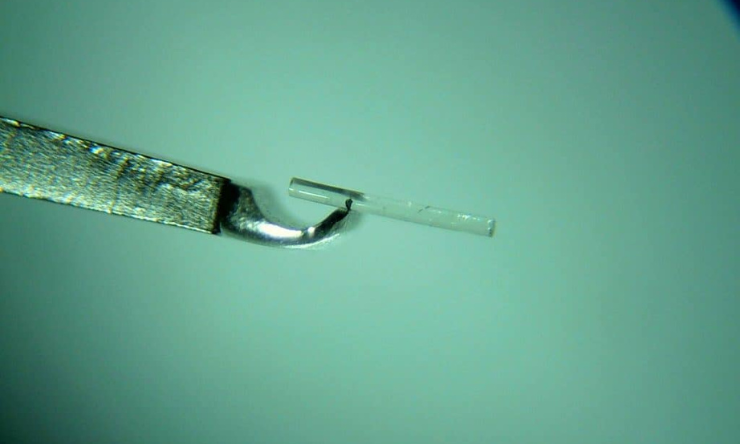
Cataracts are graded according to their location within the crystalline lens and can be anterior, posterior, sub-capsular, cortical and/or nuclear. The density, hardness or thickness of the cataract is also noted and both these classifications help to explain the symptoms that a cataract causes and how to plan surgery, which is the usual treatment. This involves removing the patient’s natural lens (which has become cloudy, resulting in visual loss) and replacing it with an artificial lens.
Apart from the usual risks of surgery, there are a few extra things that need to be considered when performing cataract surgery in patients with glaucoma. Depending on the type of glaucoma, the supporting lens structures may be weakened. This may necessitate placing the replacement artificial lens in a different location from usual and even more reinforcing surgery. Also, the pupil may not dilate well enough to gain access to the cataract. For this reason the pupil may need to be mechanically stretched during the operation. Any and all of these manoeuvres lengthen the operation and make it a little more risky.
After cataract surgery, additional medications may be used to provide adequate pressure control. These may be administered at the conclusion of surgery or maintained throughout the post-operative period. Occasionally, the pressure may jump out of control and necessitate glaucoma surgery, but more often glaucoma control is aided by cataract surgery.
Cataract surgery is not performed to rid a patient of the need to wear glasses although this may be an additional benefit of the modern customised intraocular lens (IOL) that is implanted after the cataract is removed. Although central vision will be improved by surgery, the areas of visual field that have been damaged by glaucoma cannot be improved. In fact, once the overall vision improves, some patients with severe glaucoma may become more conscious of the areas in which they cannot see (scotomas). These have not resulted from cataract surgery but from the underlying glaucoma damage. If patients have severe glaucoma, affecting the central vision, there is a risk that any surgical intervention may cause the remaining nerve fibres to die ("snuff out"). Unfortunately, this may have occurred over time with or without surgery. Fortunately, this is rare. Naturally the risks and benefits need to be discussed with your surgeon and these are calculated on an individual, case by case, basis.
In skilled hands, with appropriate preoperative and postoperative care and planning, cataract surgery, although potentially more difficult in patients with glaucoma, is still one of the most successful operations people can have. The results can be excellent and make a huge difference to a patient’s everyday quality of life and independence.